Most Americans are experiencing physical signs of stress: when you feel headaches, muscle tension, sleep disruption, or digestive issues, they signal chronic stress that elevates inflammation and raises risk of cardiovascular disease and immune dysfunction. You should know that 75% of US adults report these symptoms, and that timely action-stress management, sleep, and professional help-can be highly effective in reversing harm. Your daily habits directly influence symptoms, so apply evidence-based strategies to protect your health.
Key Takeaways:
- About 75% of adults report physical stress symptoms-headaches, fatigue, sleep disruption and muscle tension-reflecting widespread physiological impact.
- Major drivers include financial strain, work pressure, ongoing pandemic-related health concerns, with higher rates among women, younger adults and lower-income groups.
- Lack of access to mental-health care and limited workplace supports worsen outcomes; expanding care, addressing systemic stressors and promoting practical self-care (sleep, exercise, therapy) can reduce symptoms.
Understanding Stress
You experience stress as a coordinated physiological and psychological reaction that prepares you to respond to challenges; within seconds your sympathetic nervous system spikes heart rate and cortisol rises, while over time repeated activation produces physical symptoms like headaches, sleep disruption, and muscle tension-conditions reported by about 75% of adults-so you should track triggers and intensity to limit harm.
Definition of Stress
You can define stress as the body’s integrated response – behavioral, hormonal, and autonomic – to perceived demands; the HPA axis and adrenal hormones coordinate this reaction, shifting resources away from digestion and immune function toward immediate action, which explains why acute activation feels energizing but prolonged activation undermines health.
Types of Stress
You encounter several categories: acute stress lasts minutes to days, episodic acute recurs frequently, chronic persists for months or years, eustress motivates, and traumatic stress follows life-threatening events and can precipitate PTSD in roughly 7-8% of people; each type produces distinct patterns of physical and behavioral signs.
- Acute stress – short-lived response to immediate threats (e.g., a near-miss car accident).
- Episodic acute – frequent spikes from a high-pressure job or chaotic home life.
- Chronic stress – sustained demands such as caregiving or prolonged financial strain linked to immune dysregulation.
- Eustress – positive challenge that enhances performance, like an invigorating deadline.
- Perceiving Traumatic stress – exposure to life-threatening events that can lead to long-term symptoms and increased medical utilization.
| Acute | Minutes-days; triggers fight-or-flight, common symptoms: headache, tachycardia |
| Episodic acute | Repeated acute episodes; often linked to anxiety disorders and frequent somatic complaints |
| Chronic | Months-years; associated with higher risk of hypertension, metabolic changes, immune suppression |
| Eustress | Short-term positive stress that improves focus and motivation without lasting harm |
| Traumatic | Severe events; elevates PTSD risk (~7-8% lifetime), long-term sleep and pain disorders |
You should note practical examples: an exam or sprint causes acute stress, juggling multiple deadlines produces episodic acute stress, and relentless caregiving creates chronic stress that elevates inflammation markers over months; clinicians use duration and functional impact to guide interventions.
- Duration – distinguishes acute (short) from chronic (long), guiding treatment choices.
- Source – situational (work, family) versus traumatic (assault, disaster) affects recovery paths.
- Physiology – cortisol patterns, heart-rate variability, and inflammatory markers differ by type.
- Outcomes – chronic exposure predicts more comorbidities and healthcare use.
- Perceiving your stress pattern helps target behavioral, medical, or psychological strategies.
| Dimension | Clinical implication / example |
| Onset | Sudden (acute) vs. gradual (chronic); sudden events may need stabilization, chronic needs long-term management |
| Frequency | Isolated vs. recurrent – episodic patterns often co-occur with anxiety diagnoses |
| Physiological markers | Cortisol slope, HRV, CRP levels inform severity and treatment response |
| Functional impact | Work, sleep, relationships affected – guides referrals to therapy, medication, or lifestyle change |
| Recovery trajectory | Short recovery (acute/eustress) vs. prolonged recovery (traumatic/chronic) dictates follow-up intensity |

The Prevalence of Stress Among US Adults
You see the scale: 75% of US adults report physical symptoms of stress, and that aligns with broader findings – A recent survey by the American Psychological Association … – showing stress affects daily functioning. If you’re among them, you’re likely to notice headaches, muscle tension, or sleep disruption; these symptoms can raise long-term health risks such as cardiovascular strain if not addressed.
Statistical Overview
You can parse the numbers: surveys indicate 75% report at least one physical symptom like headaches or fatigue, while broader measures show up to 89% of adults say stress affects their health and behavior. Employment stress, financial worry, and caregiving are major drivers, and you likely see higher symptom counts during peaks like tax season or pandemic surges.
Demographic Variations
You notice patterns across groups: younger adults and parents report more frequent symptoms, women report physical complaints at higher rates, and lower-income adults face compounded stress from resource strain and less access to care. Regional and occupational differences matter too; for example, frontline healthcare workers often report persistent fatigue after extended shifts.
If you’re young, you may feel stress tied to job instability and social media, which correlates with sleep disruption and headaches; if you’re a caregiver or low-income, the combination of chronic stress and limited healthcare access can intensify symptoms and delay treatment. In contrast, older adults sometimes report fewer acute symptoms but carry higher baseline risk for stress-related conditions, so you should weigh symptom frequency against long-term risk.

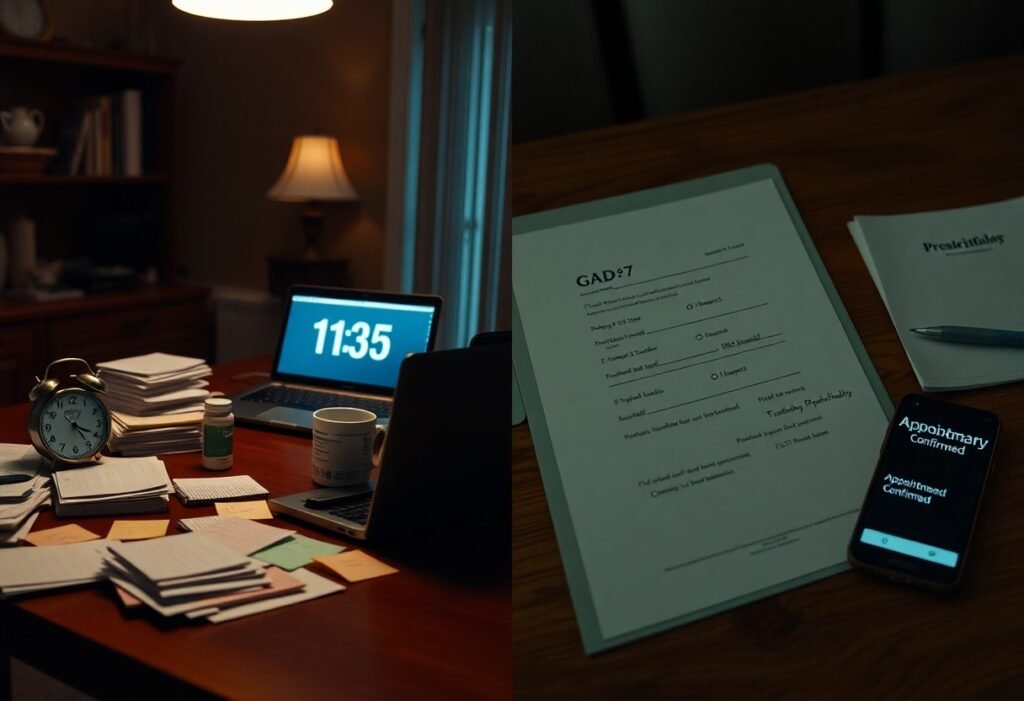
Physical Symptoms of Stress
Physical reactions often surface before you consciously identify stress: tension headaches, jaw clenching, heart palpitations, and digestive upset are common signs you shouldn’t ignore. Surveys find that about 75% of US adults report at least one stress-related physical symptom, and these signals can fluctuate with work pressures, sleep loss, or caregiving demands. Track patterns so you can address triggers early and avoid escalation into chronic problems.
Common Physical Manifestations
Headaches and muscle tension in the neck and shoulders are frequent, while many people experience insomnia, frequent indigestion, or sudden fatigue; you might also notice lightheadedness or increased frequency of colds. Symptoms vary by person and context-office workers often report neck strain, whereas parents frequently cite disrupted sleep-so use symptom clusters to identify which daily pressures are affecting your body.
Long-term Health Implications
When stress is sustained, it shifts physiology: elevated blood pressure, disrupted glucose metabolism, and heightened inflammation raise your risk of cardiovascular disease-studies link chronic work stress to roughly a 40% higher risk of coronary events-and weaken immune defenses. Left unmanaged, these changes make you more susceptible to hypertension, type 2 diabetes, and recurrent infections.
Mechanistically, repeated activation of the HPA axis and excess cortisol promote visceral fat, insulin resistance, and persistent inflammation (e.g., higher CRP). Longitudinal caregiver studies demonstrate faster health decline and shorter cellular aging markers, illustrating how ongoing stress translates into measurable, long-term biological wear that you can mitigate with interventions.
Psychological Impact of Stress
When stress becomes ongoing, it rewires how you process emotions and threats: your startle response heightens, patience thins, and mood regulation falters. Research links chronic stress to roughly a twofold increase in depressive episodes and elevated anxiety, and in high-burden groups-like caregivers and frontline workers-studies report anxiety/depression rates of 40-60%. You may also develop persistent irritability, rumination, or hypervigilance that precede full psychiatric diagnoses.
Mental Health Correlations
You’ll notice that sustained stress correlates tightly with clinical conditions: multiple cohort studies find chronic stress predicts higher incidence of anxiety and depression, more severe insomnia, and greater cognitive complaints such as poor concentration. One large population study showed individuals reporting frequent stress had about a 2x likelihood of a subsequent depressive episode versus low-stress peers, highlighting how psychological strain translates into diagnosable illness.
Behavioral Changes
Under ongoing stress, your behaviors shift in predictable ways: many people increase alcohol or tobacco use, binge or undereat, and withdraw socially-patterns that worsen outcomes. Surveys during major stressors show self-reported alcohol and substance use rises by roughly 20-30% for subsets of adults, while risky decision-making and reduced adherence to medical regimens become more common.
More specifically, you may miss deadlines, take more sick days, or show up but underperform (presenteeism); workplace studies link high stress to higher turnover and errors. Tracking your patterns-sleep loss followed by late-night eating or impulsive spending-can reveal triggers and timelines, and clarifying these sequences often exposes the behavioral loops that keep stress entrenched.

Factors Contributing to Increased Stress Levels
- Economic pressures
- Workload and job insecurity
- Health concerns
- Social isolation and digital overload
- Environmental stressors (noise, housing, climate)
Any one of these pressures can push your physiology toward chronic tension, and when several overlap your risk of sleep disruption, anxiety, or cardiovascular strain rises rapidly.
Economic Pressures
You see the impact of inflation, rising rents and mounting debt on daily decisions: approximately two-thirds of adults report finances as a top stressor and U.S. student loan debt exceeds $1.7 trillion, which fuels long-term worry. Job insecurity and unpredictable schedules make budgeting harder, so you may cut health appointments or skip sleep to work more-both of which amplify physiological stress responses and hinder recovery.
Social and Environmental Influences
Your social environment and surroundings shape stress: about 72% of adults use social media, exposing you to constant comparisons and negative news, while poor housing, neighborhood noise, and limited green space elevate daily tension. Community violence or isolation increases vigilance and raises cortisol levels, so even routine errands can feel threatening and erode resilience over time.
Digging deeper, physical environment factors produce measurable effects: a 2019 study linked spending at least 120 minutes per week in nature to improved well-being for many participants, while chronic noise exposure has been associated with higher blood pressure and sleep fragmentation in urban cohorts. You experience these influences cumulatively-lack of green space, crowded housing, and continuous digital alerts together sustain hyperarousal and make recovery harder.
Managing Stress Effectively
Coping Strategies
You can reduce physical symptoms by combining quick interventions and routine habits: practice diaphragmatic breathing for 5-10 minutes to lower heart rate, do 30 minutes of moderate exercise most days to cut stress hormones, and use progressive muscle relaxation to release tension in 10-15 minutes. Set clear boundaries at work, limit screen time an hour before bed, and track sleep toward 7-9 hours nightly to blunt chronic activation.
Professional Help and Resources
If symptoms persist or impair daily life, seek evidence-based care: CBT and MBSR reliably reduce anxiety and stress-related symptoms over 6-12 weekly sessions, while a psychiatrist can evaluate medications for severe cases. Get immediate help for chest pain, fainting, or suicidal thoughts-these are medical emergencies that need urgent attention.
Use the SAMHSA treatment locator or therapist directories to find in-network providers; many employers offer Employee Assistance Programs and teletherapy platforms expand access. In crisis, call 988 for suicide or mental-health emergencies or SAMHSA’s helpline at 1-800-662-HELP for treatment referrals and local resources.
To wrap up
High rates of stress-related physical symptoms stem from chronic pressures, lifestyle limits, and limited access to care. Sleep, diet, and activity levels interact with work and financial strain to cause headaches, muscle tension, and fatigue. Pervasive social and tech-driven demands amplify these physical responses. Prioritize manageable coping strategies, seek professional support when needed, and advocate for systemic changes that reduce burdens on individuals.
FAQ
Q: Why do about 75% of US adults report physical symptoms of stress?
A: Multiple factors explain why many adults experience physical stress symptoms. Chronic stress raises cortisol and adrenaline, leading to headaches, muscle tension, digestive issues, sleep disruption, and fatigue. Social drivers like financial insecurity, job pressure, caregiving, isolation, and constant news exposure increase daily stress. Limited access to affordable mental health care and time constraints reduce healthy behaviors. This makes recovery difficult, so transient stress becomes chronic and manifests physically.
Q: What specific physical symptoms are most commonly reported and why do they occur?
A: Common stress symptoms include tension headaches, neck and back tightness, chest pain or palpitations, and gastrointestinal issues like nausea or stomach pain. Fatigue, sleep problems, and increased infections or skin flare-ups are also frequent. Stress hormones alter blood flow, raise muscle tension, disrupt digestion, impair sleep, and suppress immunity. Behavioral changes such as poor diet, less exercise, and more alcohol or nicotine use can further amplify these symptoms.
Q: How do workplace and economic conditions specifically drive physical stress responses?
A: Job insecurity, long hours, high demands with low control, tight deadlines, unpaid overtime, and precarious gig work all fuel chronic stress. Financial strain and balancing paid work with unpaid caregiving increase stress and reduce recovery time. Commuting, harassment, or unsupportive management add to physiological strain. Over time, this repeated wear and tear leads to pain, fatigue, sleep issues, and digestive problems.
Q: When should physical symptoms that may be stress-related prompt medical evaluation?
A: Seek immediate care for sudden, severe symptoms. These include chest pain, fainting, shortness of breath, sudden numbness, high fever, or vomiting blood. Schedule a prompt appointment for persistent or worsening issues that disrupt daily life. This includes mood changes, suicidal thoughts, or major sleep problems. A clinician can rule out medical causes. They can also assess for anxiety or depression. Finally, they can connect you to therapy, medication, or community resources.
Q: What evidence-based steps can reduce physical symptoms of stress for most people?
A: Effective strategies include improving sleep regularity and duration. Engage in regular moderate aerobic exercise. Practice daily relaxation techniques like deep breathing or mindfulness. Reduce stimulants and excess alcohol. Maintain regular meals.
Cognitive-behavioral therapy and stress-management programs reduce symptoms. Short therapy courses or digital CBT are accessible options. Strengthen social support and set work boundaries. Use time-management and problem-solving skills. Seek workplace accommodations when needed.
If symptoms persist, coordinate care with primary and mental health providers.